How is Prostate Cancer Diagnosed?
Diagnosis of prostate cancer is a four-step process. If the PSA levels in your blood test suggest the possibility that you may have prostate cancer, your physician will order a biopsy. If there is cancer present in the biopsy samples, it will be given a Gleason score and stage-two numbers that indicate the extent and aggressiveness of the cancer.
Step 1: Testing for Elevated PSA Levels
Your prostate cancer screening includes a test to measure the levels of prostate-specific antigen (PSA) in your blood. Elevated PSA levels are often an early indication of prostate cancer as well as other prostate disorders.
PSA is a protein produced by the prostate that helps keep semen liquid outside the body. When the prostate is healthy, a very small amount of PSA escapes from the prostate and enters the bloodstream. When the prostate is unhealthy-if it is inflamed, enlarged or contains cancerous cells-larger amounts of PSA leak into the bloodstream.
PSA levels of 4ng/ml and above are considered elevated, however, there is no specific level that indicates cancer. Results from regular PSA screenings will show whether your PSA levels have changed year to year, and whether that change is cause for concern.
Step 2: Prostate biopsy
 While the PSA test helps assess the risk of prostate cancer, the prostate
biopsy is the only way to make an accurate diagnosis. If either your digital
rectal exam or blood test had an abnormal result, your physician will
often order a biopsy.
While the PSA test helps assess the risk of prostate cancer, the prostate
biopsy is the only way to make an accurate diagnosis. If either your digital
rectal exam or blood test had an abnormal result, your physician will
often order a biopsy.
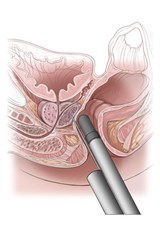
What To Expect During A Prostate Biopsy
Your biopsy will be performed by a urologist in an outpatient surgery center. The entire procedure usually takes about 15 minutes or less and you'll receive a local anesthetic for minimal discomfort. While lying on your side, an ultrasound probe will be inserted into the rectum. This probe provides a clear visual of the prostate and allows the physician to guide the very fine biopsy needle into the prostate.
Using the needle, the physician will take tiny tissue samples-called cores-from different areas of the prostate. These cores are the width of only four threads. The samples are sent to a uropathologist, who determines if there is cancer present. If cancer is present, the uropathologist gives the cancer a Gleason score.
Step 3: Assessing your Gleason score
The Gleason score is a number given by the pathologist who examines the cancerous tissue samples under a microscope. The Gleason score refers to how different the prostate cancer cells/glands appear in comparison to normal prostate cells/glands. The pathologist provides two grades, or numbers, based on the pattern of cancer cells/glands that appear under the microscope. Each grade is based on a scale of 1 to 5. The two grades are added together for your Gleason Score. With today's biopsy methods/grading recommendations, almost all prostate cancer patients have a Gleason Score of 6 or above. These scores are then rated into low-risk (≤6), intermediate (7) and high-risk (8, 9, or 10) categories.

Step 4: Staging the Prostate Cancer
Prostate cancer is also assigned a stage, based on how advanced the disease is. Both your Gleason score and stage are critical deciding factors in what types of prostate cancer treatment may be recommended. See treatment options for early stage prostate cancer or treatment options for advanced stage prostate cancer.
The clinical stages of prostate cancer:
- T1: The earliest stage is divided into three types: T1a, T1b, and T1c.
- T1a is when prostate cancer is found during a surgery performed on the prostate for an unrelated condition. It is microscopic and found in less than 5 percent of the prostate tissue.
- T1b is found similarly to T1a, but the cancer is more extensive, involving more than 5 percent of the tissue.
- T1c is the most frequently found prostate cancer. It is detected by a prostate biopsy, which was done because of information provided by PSA testing.
- T2: The cancer is still entirely within the prostate, but T2 cancer can be felt during a digital rectal exam.
- T3: The cancer has begun to spread locally beyond the prostate but has not reached the lymph nodes.
- T4: The cancer has spread and may have reached the bladder, the rectum, or other nearby areas of the body, including the lymph nodes and/or the bones.
